Top Tips for Avoiding Unnecessary Thyroid Surgery
After being given the diagnosis of "Thyroid Nodule", a whirlwind journey starts which can sometimes result in unnecessary thyroid surgery. One that includes diagnostic testing such as ultrasounds, so called "biopsies" which are done with a needle, and results which can all sound "suspicious". If that isn't enough, the journey may end with a decision for Thyroid Surgery: removing part or all of the thyroid gland. That procedure is not without inherent risks. Whilst I have performed that procedure countless times, every time I walk into an operating room, I enter with the respect that my hands have the power not only to help someone, but also to hurt someone. Thankfully, there are many well trained thyroid surgeons like myself all over the globe, but even in the best of hands misfortune can occur despite the best of circumstances. For that reason, it only makes sense that the commitment to undergo surgery should be intentional and one of informed consent. In my experience, I have unfortunately had the misfortune of consulting on people who had thyroid surgery that went bad. A few who saw a surgeon, had the workup and got persuaded into having surgery for something that did not appear cancerous from the onset. The recipient of the surgery, however, may not have fully understood but got signed up for surgical management nonetheless. The resulting hoarseness or hormonal problems that arise after a complication has occurred can be difficult to manage, and may not have happened if the following steps had been followed:
- The details of the thyroid nodule must be understood. Unfortunately, to fully understand what is going on there is an acquisition of knowledge that needs to occur. A doctor taking insurance will likely only spend the 8 minutes allotted to discuss the case and risks with you. That will never be enough time to fully comprehend all aspects of a thyroid nodule and its nuances in treatment. While commitment to surgery does not require the level of understanding of a thyroid surgeon, there is a bare minimum that should be present to make informed consent to surgery. The first is understanding the "why" surgery is needed. This includes understanding the percentage risk of actually having Thyroid Cancer and what is the goal of the surgery. Oftentimes, the goal of the surgery is perceived as eliminating a symptom which has been assumed to be because of a thyroid nodule. Sadly, this is mostly not the case.
- Learn how the process of getting a diagnosis works - Study the Thyroid Nodule Mindmap to see the process from beginning to end, with all the options and variations.
- Understand what the actual biopsy results mean - There are many different results with different meanings. While we use the term "needle biopsy", these are not true biopsies because there is no "chunk" of tissue. It is really cytology, which means a spattering of cells. This has its own limitations which can often times be translated into lay people terms that end up sounding more suspicious than they really are. The most confusing nodule of them all is the "Indeterminate Nodule" which is the most common reason people may have unnecessary thyroid surgery. Master understanding this nodule to lower risk of unnecessary surgery.
- Once the above is well understood, make sure the workup has been performed fully enough for a decision for surgery to be made. Sometimes unnecessary thyroid surgery can directly proceed a "non-diagnostic" result on needle biopsy, just because the diagnosis is completely unknown. Remember that most nodules (80-85%) are benign. An operation may be appropriate in these instances, however, the completeness of the workup is not only for the doctor to decide. If the person deciding on surgery isn't convinced of the reason or need, options don't have to be skipped to go directly to surgery. Repeat fine needle aspiration or molecular genetics can be performed to make the decision more informed. When uncertain, a second opinion can sometimes help reveal the completeness of the workup and/or steps that may have been skipped that could be considered before committing to surgery.
- After all of the above has been absorbed, and the decision for thyroid surgery is made, there are a few important considerations to be made about "who" is going to do the surgery. Low volume thyroid surgeons account for most of the surgical complications that arise. The great variation in nerve anatomy and parathyroid location and identification while performing surgery, require skill to achieve consistent positive outcomes. Being the exception to the rule may be a low thyroid surgeon's first complication, mainly because they are just not that familiar with the particular anomaly at hand.
The 10 questions that should be asked to assess the surgeon's expertise are:
- "How many surgeries do you do a year?"
- Typically, surgeons who perform 25 or more thyroid surgeries a year have the lowest complication rates. Unfortunately, 50% of thyroid surgeons perform only one or a few cases per year. Having unnecessary thyroid surgery in the hands of a low volume thyroid surgeon can have the makings of a very unfortunate outcome.
- "How many surgeries have you performed in your career?"
- It is said that an experienced thyroid surgeon has performed 500 or more thyroidectomies to become proficient. While this number is not a hard requirement, a few many hundreds should be considered to assess sufficient experience.
- "What are the risks of thyroid surgery?"
- This explanation should include Recurrent Laryngeal Nerve injury causing hoarseness and swallowing problems, parathyroid gland injury causing low calcium and need for medications to maintain calcium, as well as the standard risks of surgery. Tracheostomy, while extremely rare, if mentioned shows the level of completeness and transparency that should be comforting and not alarming. If these are not explained or mentioned in some fashion, then informed consent is not really being obtained.
- "What is your complication rate of these risks?"
- If this question shakes the surgeon, it is because few people ask it. Pay attention to the surgeon's response. The rate of nerve injury in experienced hands is considered at 1% for first time surgery and 10% for revision surgery. Most surgeons will just quote these numbers, hopefully because they don't have any complications. But if you are with a high volume surgeon, they will eventually meet a difficult case that a complication is unavoidable. When the surgeon says the rate is 1%, a good followup is "have you even had this complication?" pushing for their own specific rate rather than what is published. It should be noted that sometimes these complications are just temporary and not permanent. A tranparent surgeon will mention that they have some of these complications which are mostly temporary and reverse with time. Just know that even the world famous surgeons have had some of the complications, but that doesn't mean they aren't fit to do surgery.
- "How much of my thyroid are you going to remove?"
- Be clear on how much thyroid is planned to be removed from the beginning. Understand the pros and cons of starting with half versus whole removal.
- "Will there be an intraoperative pathology consultation and how will the results change the surgery?"
- As the approach to partial thyroid removal is generally half possible whole based on "frozen section" or intraoperative pathology consultation, it is important to know if this is plan and how the surgeon plans to use the results to decide upon removing the whole gland.
- "Does this treatment follow published guidelines?"
- Guidelines are changing for less aggressive management of thyroid cancer in particular cases. If the surgeon mentions the American Thyroid Association (ATA) Guidelines based on a particular year, these tend to be the most followed guidelines. While guidelines are there as a reference, many times the best option may be to not follow the guidelines. If there is interest in not following guidelines, there generally should be reasons and research that support such an approach.
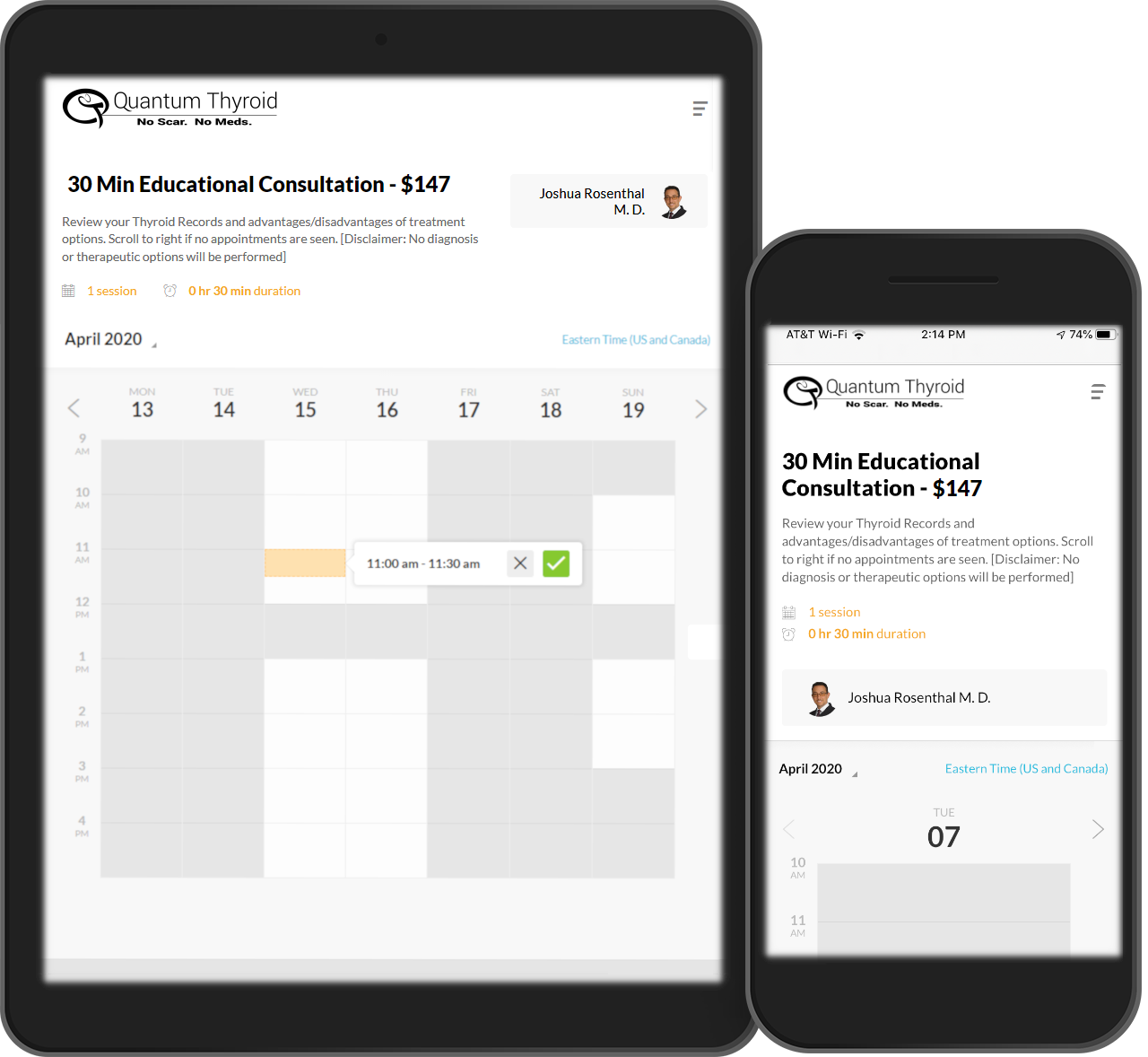
- "Are there any other options other than surgery?"
- Surgeons often don't mention options other than surgery. When non-surgical and less invasive options are mentioned, informed consent is being obtained. There are even a few options for surgical technique and approach, but these are usually chosen by patients who seek out a surgeon performing that unique technique.
- "Who, other than you, will actually be performing the surgery?"
- Sometimes the attending surgeon will be assisted by surgical fellows or residents. Many times the attending surgeon may have more than one case going on and may jump from room to room. It is important to know if the surgeon who you are talking to is the only surgeon who will be operating and if he will be present the entire procedure.
- "Will there be a scar and how big will it be?"
- Unless you are getting a newer procedure, surgery almost always includes a scar. The scar may be placed in unusual areas such as the armpit, the mouth/under lip, or even camouflaged like a face-lift. Generally, standard operating procedure is through the neck along natural skin creases and only needs to be about 1-2 inches at most. This can yield fantastic results. Ask to see some pictures of what you might expect if you are concerned.